redo Jump to...
print Print...

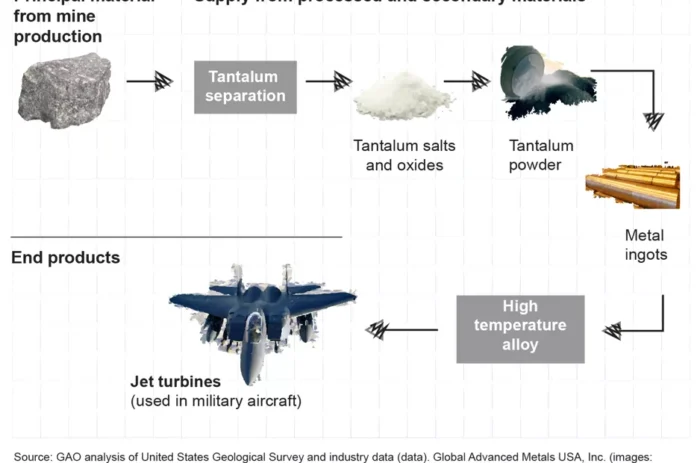
The highest standard used in West Africa is a hooded coverall. It is used by Medecins Sans Frontieres. The material used is not ordinary plastic. It is tested to be resistant to contagious liquids such as blood and vomit.

(Photo: CBS News, Dallas-Fort Worth)
(by Ashley Fantz and Holly Yan, CNN) – A day after the Centers for Disease Control and Prevention (CDC) said a Texas health care worker tested positive for Ebola, health officials are still trying to figure out how exactly she caught it.
“Something went wrong, and we need to find out why and what,” said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases.
The woman, identified by CNN affiliate WFAA as Nina Pham, took basic precautions while treating an Ebola-stricken Liberian national at a Dallas hospital. Now she is the first person to have contracted the deadly virus in the United States.
There are few details that are known about what might have gone wrong. She wore a mask, gown, shield and gloves when treating Thomas Eric Duncan, who was in isolation at Texas Health Presbyterian Hospital, officials said.
But on Monday, Dr. Tom Frieden, director of the CDC, told reporters that it’s still unknown how the infection occurred, only that a “breach in protocol” for treating a patient happened.
CDC Director Tom Frieden (Photo: NBC News)
Frieden said state and federal health officials are re-examining those protocols, including the removal of protective gear after contact with an Ebola patient and if it might be helpful to spray virus-killing solution on workers as they leave an isolation unit. He said Monday that the nurse is “clinically stable.”
How did it happen?
On Monday morning, an official with direct knowledge of the Texas nurse’s case told CNN that CDC disease detectives interviewed the nurse several times and thought there were “inconsistencies” in the type of personal protective gear she wore and with the process used to put the gear on and remove it.
Frieden has spoken of possible ways she became infected. It could have happened when the nurse removed her protective gear — a bit of infected bodily fluid somehow touching her — or it she could have come into contact with infected fluid as Duncan received kidney dialysis or respiratory intubation.
Those procedures were “a desperate measure to try to save his life,” Frieden said. “Both of those procedures may spread contaminated materials and are considered high-risk procedures.”
He said, “When you have potentially soiled or contaminated gloves or masks or other things, to remove those without any risk of any contaminated material … touching you and being then on your clothes or face or skin … is not easy to do right.”
Or the problem could have been something else entirely.

….The CDC concedes the Texas nurse’s case is worrisome. “It is possible in the coming days that we will see additional cases of Ebola,” Frieden said.
That’s because others who provided care to Duncan could have had the same kind of breach as the infected nurse. The CDC is still working to compile a list of health care workers who were involved in Duncan’s care from September 28 to October 8, the day he died, an official with direct knowledge of the Texas case told CNN on Monday.
The official added that the health care workers who have been identified will be visited twice daily to be checked for fever, one of the symptoms of Ebola. Those workers had previously been self-monitoring, the official said, because they were not — before the Texas nurse tested positive — considered high-risk.
In addition, the public areas of the nurse’s apartment complex have been decontaminated and her neighbors have been notified. The city of Dallas made a reverse 911 call to residents in the area, telling them about the city’s second Ebola case.
“I think it needs to be put into context that … you can’t make an extrapolation that this is now a danger more so to the American people,” said Dr. Anthony Fauci, director of the National Institute of Allergy and Infectious Diseases.
But fear is spreading.
When a passenger on a flight from New York to Los Angeles fell ill Sunday, the biggest concern was Ebola. The plane was taken to a remote gate at Los Angeles International Airport. After a few hours, officials determined the woman did not appear to have Ebola, and other passengers were allowed to leave.
And in Louisiana, Attorney General Buddy Caldwell plans to seek a temporary restraining order to block the disposal of incinerated waste from Duncan’s personal items at a Louisiana landfill.
“There are too many unknowns at this point, and it is absurd to transport potentially hazardous Ebola waste across state lines,” Caldwell said Sunday.
CNN’s Catherine E. Shoichet contributed to this report. Reprinted here for educational purposes only. May not be reproduced on other websites without permission from CNN. Visit the website at cnn .com.
Questions
1. What precautions did the Dallas nurse who contracted Ebola take?
2. What does CDC director Dr. Thomas Frieden say about how the infection occurred?
3. a) What additional steps is the CDC considering telling health care workers to take?
b) Is there any reason why they shouldn’t be doing this already, or at all? Explain your answer.
4. What did the CDC “disease detectives” who interviewed the nurse, Nina Pham, discover about the steps she took before/after treating the Ebola patient who died?
5. What possible ways might Ms. Pham have become infected, according to CDC director Dr. Tom Frieden?
6. CDC director Dr. Tom Frieden said, “When you have potentially soiled or contaminated gloves or masks or other things, to remove those without any risk of any contaminated material…touching you and being then on your clothes or face or skin…is not easy to do right.” If he knows this to be true, does the CDC have any responsibility to better train health care workers? And what, if anything, should he have done when it was announced that Thomas Duncan was admitted to the Texas hospital with Ebola?
7. The CDC has an $11 BILLION annual budget. Consider the following: Do you think the agency is doing all they can to prevent further outbreak? Should they be monitoring treatment of the few known Ebola patients in the U.S., or leave it up to the hospitals? Is it the role of this government to take a “hands-on” approach to ensure proper protocol? Should CDC director Dr. Frieden establish a better system for the treatment of Ebola? Explain your answers.
CHALLENGE QUESTION:
The acronym CDC stands for Centers for Disease Control and Prevention.
Do some research to find out what this $11 billion government agency is doing to prevent the spread of Ebola in the United States. Explain what methods of prevention you have found. Do you feel the CDC is doing enough to prevent the spread of Ebola in the U.S.?
Background
The National Institutes of Health (NIH) is an agency of the U.S. Department of Health and Human Services and is the primary agency of the United States government responsible for biomedical and health-related research.
The National Institute of Allergy and Infectious Diseases (NIAID) is one of the 27 institutes and centers that make up the National Institutes of Health (NIH), an agency of the Department of Health and Human Services (HHS). NIAID’s mission is to conduct basic and applied research to better understand, treat, and prevent infectious, immunologic, and allergic diseases.
NIAID has “intramural” (in-house) laboratories in Maryland and Montana, and funds research conducted by scientists at institutions in the United States and throughout the world. NIAID also works closely with partners in academia, industry, government, and non-governmental organizations in multifaceted and multidisciplinary efforts to address emerging health challenges such as the pandemic H1N1/09 virus.
The Centers for Disease Control and Prevention (CDC) is the U.S.’s national public health institute. It is a federal agency under the Department of Health and Human Services.
- Its main goal is to protect public health and safety through the control and prevention of disease, injury, and disability.
- The CDC focuses national attention on developing and applying disease control and prevention.
- It especially focuses its attention on infectious disease, food borne pathogens, environmental health, occupational safety and health, health promotion, injury prevention and educational activities designed to improve the health of United States citizens.
- CDC’s 2014 budget is $11.3 billion.
- CDC’s Ebola webpage at: cdc.gov/vhf/ebola/index.html
CNN reports: CDC Director Dr. Thomas Frieden said a “breach in protocol” led to the nurse becoming infected with Ebola. So what’s the protocol for health care workers if they suspect a patient has the virus that has already killed more than 4,000 people in West Africa?
Go through the checklist
- Signs of an Ebola infection include fever, headache, vomiting, diarrhea, muscle pain or bleeding, according to the Centers for Disease Control and Prevention. But a key clue is whether the person traveled to an Ebola-affected area — such as Sierra Leone, Liberia or Guinea — in the past three weeks. That’s because the symptoms of Ebola can take anywhere from two to 21 days to show up.
Isolate the patient
- Once Ebola is suspected, the patient should get his or own room, with a private bathroom, the CDC said. And the door to the hallway should remain closed.
- Hospitals should maintain a log of everyone who enters the room, the agency said.
- It’s also a good idea to keep someone stationed at the patient’s door to make sure everyone going in is wearing the right protective equipment.
Get the right gear
- At the very least, those who enter the patient’s room should wear gloves, a gown, eye protection and a face mask.
- Sometimes the situation calls for more precautions, such as wearing disposable shoe covers, leg covers and two layers of gloves.
- Those extra steps are needed if there is vomit, human waste or “copious amounts of blood” in the room, the CDC said.
Know the right order
- It’s not enough to have protective clothing; putting it on in the right order is just as important.
- “The dressing and undressing of (protective wear) should be supervised by another trained member of the team,” the World Health Organization advises.
- After donning scrubs, health care workers should put on either boots or closed, water-resistant shoes with overshoes.
- Then a waterproof gown should go over the scrubs. If one isn’t available, wear a waterproof apron over a gown.
- Next come the face mask, goggles and a head cover, if available.
- Finally, after washing their hands, health care workers should put on gloves over the sleeves’ cuffs.
- When it’s time to take the gear off, extreme care must be taken to avoid contaminating regular clothing, eyes or mucous membranes.
- CDC Director Dr. Tom Frieden said gear removal is a “major potential area for risk.”
- “When you have gone into and potentially soiled or contaminated gloves or masks or other things, to remove those without any risk of any contaminated material touching you and being then on your clothes or face or skin and leading to an infection is critically important and not easy to do right,” Frieden said.
Keep visitors out
- It may seem obvious, but it’s important to keep visitors away from the patient’s room.
- “Exceptions may be considered on a case-by-case basis for those who are essential for the patient’s well-being,” the CDC said.
- Keeping visitors away doesn’t just protect them; it also protects hospital workers, patients and others in case the visitor may have contracted Ebola, too.
- Those who do visit should be screened for fever and other symptoms.
- All these procedures may seem tedious, but every precaution matters, Frieden said.
- “The care of Ebola can be done safely, but it’s hard to do it safely. It requires meticulous and scrupulous attention to infection control, and even a single, innocent, inadvertent slip can result in contamination.”
Resources
Dr Daniel Varga, chief clinical officer at Texas Health Presbyterian Hospital where the worker was infected, answers journalists’ questions at a news conference in Dallas (10/12/14):
Daily “Answers” emails are provided for Daily News Articles, Tuesday’s World Events and Friday’s News Quiz.